Key Takeaways
1. Suicide: A Pervasive and Misunderstood Crisis
Death, as Seneca states, has always lain close at hand; yet it is a mystery why the first to kill himself did: Was it a sudden impulse, or prolonged disease?
An ancient problem. Suicide has been a part of human history for millennia, with societal attitudes shifting from acceptance to condemnation, and eventually to understanding it as a consequence of mental illness. Despite its long history, the act remains deeply complex and often inexplicable.
A modern epidemic. In recent decades, suicide has become a major public health crisis, particularly among the young. It is the third leading cause of death for young people in the United States and the second for college students, with rates tripling over the past 45 years. This toll surpasses deaths from the Vietnam War and HIV/AIDS in young men.
Preventable tragedy. While the reasons for this increase are multifaceted—including easier access to lethal means, substance abuse, and earlier onset of mental illnesses—the most crucial takeaway is that most suicides are preventable. The gap between what we know and what we do is lethal, highlighting an urgent need for greater awareness and intervention.
2. Mental Illness: The Overwhelming Driver of Suicide
Indeed, in all of the major investigations to date, 90 to 95 percent of people who committed suicide had a diagnosable psychiatric illness.
Ubiquitous psychopathology. The most common element in suicide is mental illness, with mood disorders (depression and manic-depression), schizophrenia, borderline and antisocial personality disorders, alcoholism, and drug abuse being particularly implicated. These conditions are present in 90-95% of completed suicides.
High-risk conditions:
- Previous suicide attempt: 38 times the expected risk.
- Depression or prescription drug dependence: 20 times the expected risk.
- Manic-depressive illness: 15 times the expected risk.
- Schizophrenia: 8 times the expected risk.
Physical illness's role. While physical illnesses are common in suicide victims, they rarely act as a sole cause. Instead, they typically co-occur with an underlying psychiatric condition, especially those affecting the brain, such as temporal lobe epilepsy or HIV/AIDS.
3. The Psychology of Despair: Hopelessness and Impulsivity
In short, when people are suicidal, their thinking is paralyzed, their options appear spare or nonexistent, their mood is despairing, and hopelessness permeates their entire mental domain.
A private anguish. Suicide is an intensely private act, often driven by unbearable mental pain that is difficult to articulate. Suicide notes, left by only about one in four individuals, often reflect this constricted, despairing state rather than offering profound insights.
Cognitive constriction. Depression profoundly impairs cognitive function, leading to slowed thinking, distraction, and a pervasive sense of hopelessness. This mental state narrows perceived options, making death seem like the only alternative. Hopelessness is a consistent and potent predictor of eventual suicide.
Volatile states. Mania, characterized by exultant mood, racing thoughts, and impulsivity, can also be laced with irritability and paranoia, especially in "mixed states" where depressive and manic symptoms coexist. These volatile, agitated conditions are particularly dangerous, increasing the likelihood of impulsive and violent suicidal acts.
4. Biology's Role: Genes, Brain Chemistry, and Vulnerability
So potent in fact is the influence of hereditary transmission in the production of suicide, that not less than one-sixth of all recorded cases have been directly traced to this source.
Familial patterns. Suicide and mental illness often run in families, a fact observed for centuries and supported by modern research. Family, twin, and adoption studies consistently show a strong genetic influence on suicidal behavior, suggesting a biological predisposition.
Serotonin's influence. Brain chemistry plays a critical role, with serotonin being a key neurotransmitter implicated in mood, aggression, and impulsivity. Low levels of its metabolite, 5-HIAA, are consistently associated with increased suicide risk across various psychiatric diagnoses.
Stress-diathesis model. Suicide often results from a "two-hit" model: a genetic or biological predisposition (diathesis) combined with environmental triggers (stress). These triggers can include psychiatric illness, acute intoxication, personal crises, or even sleep loss, which can profoundly alter brain chemistry and lower the suicide threshold.
5. Lethal Means and Contagion: Amplifying the Risk
Suicide, dangerously, has a contagious aspect; it has, as well, for the vulnerable, an indisputable appeal as the solution of last resort.
Method matters. The choice of suicide method is influenced by availability, perceived deadliness, and cultural factors. Firearms are the leading method in the U.S., while pesticides are common in rural China. Women tend to use less violent means, though this is changing.
Contagion effect. Suicide can be contagious, especially among the young, a phenomenon known as the "Werther effect." Highly publicized or romanticized suicides, whether in literature or media, can lead to clusters of imitative deaths.
Preventing access. Limiting access to lethal means is a proven prevention strategy. Examples include:
- Detoxifying domestic gas.
- Restricting access to deadly drugs.
- Implementing gun control measures.
- Erecting barriers at popular suicide sites like bridges.
These measures can reduce overall suicide rates, as individuals do not always simply substitute one method for another.
6. Effective Treatments: Hope Through Medicine and Therapy
Lithium … is the lightest of the solid elements and it is perhaps not surprising that it should in consequence possess certain modest magical qualities.
Lithium's power. Lithium is the most effective and well-documented antisuicide medication available, reducing the risk of suicide or attempts by nearly nine times in mood disorder patients. Its efficacy stems from its mood-stabilizing effects and its impact on brain chemistry, particularly serotonin.
Beyond lithium. Other medications, including antidepressants (especially SSRIs) and antipsychotics, also play crucial roles in treating the underlying mental illnesses that drive suicide. Electroconvulsive therapy (ECT) offers rapid, life-saving relief for severe, acute depression.
Integrated care. Psychotherapy, especially when combined with medication, is vital for long-term recovery. It helps patients manage psychological pain, develop coping skills, and address treatment noncompliance, which is a pervasive and dangerous problem in chronic illness.
7. Societal Barriers: Stigma, Ignorance, and Inaction
We don’t even like to talk about it. We’ve got to change the way America feels about depression.
The stigma of illness. Societal stigma surrounding mental illness and suicide remains a significant barrier to prevention. Prominent figures like John Wilson, a D.C. Council chairman, refused hospitalization due to fears of political suicide, ultimately leading to his death by suicide.
Healthcare gaps. Doctors themselves have higher suicide rates and often struggle to seek help. General practitioners frequently underdiagnose and undertreat depression, and mental health services are often inaccessible or unaffordable.
Public health initiatives. National strategies, like the U.S. Surgeon General's Report on Suicide, advocate for increased public awareness, improved clinical services, and reduced access to lethal means. School-based programs, while well-intentioned, must be carefully designed to avoid normalizing suicide or exaggerating its incidence.
8. The Enduring Scar: Grief for Those Left Behind
Suicide is a death like no other, and those who are left behind to struggle with it must confront a pain like no other.
Profound impact. Suicide leaves survivors—parents, children, spouses, friends—with unique and devastating grief, guilt, and anger. The sudden, often violent nature of the death, coupled with police involvement and societal stigma, compounds their suffering.
Unanswered questions. Survivors are haunted by "what if's" and an agonizing need to understand "why." The absolute hopelessness of the suicidal mind often means the decision to die is tangential to the well-being of others, leaving loved ones feeling personally rejected.
Healing and advocacy. While the healing process is long and arduous, support groups and advocacy organizations provide invaluable resources for survivors. Many channel their grief into raising awareness about mental illness and suicide prevention, striving to redeem some good from their profound loss.
Last updated:
Review Summary
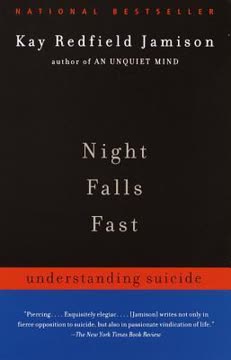
Night Falls Fast by Kay Redfield Jamison receives strong praise for its comprehensive, scientifically rigorous exploration of suicide. Reviewers appreciate Jamison's accessible writing style, her combination of clinical research with personal narratives, and her courage in addressing her own suicide attempt. The book examines suicide's biological, psychological, and social dimensions, emphasizing its strong link to mental illness. Some readers found it emotionally difficult, with warnings that it may not suit those currently experiencing suicidal thoughts. Critics note outdated information and heavy reliance on statistics. Overall, it's considered essential reading for understanding suicide as a public health crisis.
Similar Books